Muscle Strains
A muscle strain or “pulled muscle” is a common injury that happens when muscle fibers rupture as a result of mechanical stress. Although often seen in hamstrings, quadriceps, calves, rotator cuff muscles and back, a strain can happen in any muscle of the body.
Depending on the severity of the tear, we can classify strains by 3 categories:
What Causes a Strained Muscle?
Muscle strains occur when the stress applied is greater than the capacity of the muscle in that moment in time. This overload can be the result of stretching a muscle beyond its ability to contract or engaging in a powerful contraction that the muscle was not ready for.
It is important to know that anyone can suffer a muscular strain. For example, if a person has muscular weakness from a previous injury or increased muscular tension, their movement patterns can be altered, making them prone to muscle strains when performing regular activities.
Athletes involved in sports that require rapid and explosive movements can often endure strains if they are not properly warmed up or conditioned for the activity.
Other contributing factors include extreme cold temperatures, poor biomechanics, underlying health conditions as it can decrease the health and extensibility of muscles tissue.
How Can Physiotherapy, Chiropractic and Massage Therapy Help a Muscle Strain?
A customized treatment plan is key to the recovery of a muscle strain. Physiotherapists, Chiropractors and Massage Therapists are trained professionals that can help you diagnose the injury and rehabilitate it. They do this by helping you to manage pain, decrease muscular tension, increase mobility and develop the strength necessary to return to your regular activities. In addition to this, they will provide you with strategies to prevent strains from happening again.
What Should be Avoided with a Muscle Strain?
If you suspect that you have a muscle strain, it is best to consult with your Physiotherapist, Chiropractor or Registered Massage Therapist. As a rule of thumb avoid the following:
How Long Does it Take to Recover from a Muscle Strain?
Recovery will vary depending on the area affected and the severity of the injury. Other factors including age, physical demands and access to care can impact the recovery time of an individual as well.
Generally speaking, a grade 1 strain can heal in 2-3 weeks, a grade 2 can take 4-8 weeks and a grade 3 can take 5-6 months or longer.
It is important to note that if not healed properly, muscle strains can re-occur or lead to more complex musculoskeletal injuries or dysfunctions as it will impact other areas of the body.
What are some Safe Exercises to do for Muscle Strains?
Every strain and every person is different, therefore the exercise protocol will be dependent of the affected muscle group and the severity of the injury. A physiotherapist and/or chiropractor will be the best person to determine what is the most appropriate course of action in every case.
In the acute stages of healing performing active movement in a pain free range is a great way to maintain range of motion and decrease pain. As time progresses, introducing low – moderate intensity eccentric loading progressing to isotonic loading of the muscle will help increase strength. Once you have strengthened the muscle you will be ready for more complex movement patterns that are activity specific.
Remember, when dealing with any injury it is important to be patient to allow the body to heal properly. Your body is very smart and wants to get better. With proper treatment, the chances of recovery are very promising.
If you suspect that you have a muscle strain, at Sunup Physiotherapy you will find a team of highly qualified Physiotherapists, Chiropractors, and Massage therapists that will be happy to guide you in your road to recovery. Contact us today and get on the road to recovery.
Tendinopathy
A tendon is a tough band of fibrous connective tissue made of collagen fibres that connect muscle to bone. They transmit forces from muscle to bone and as such have to be capable of withstanding tension. Due to the pressure we often put on our tendons to withstand great tensile stresses, tendon injuries are among the most common overuse injuries we see in the clinic.
Tendinopathy is a broad term for a tendon injury with damage to the collagen fibres. Tendinitis (or tendinosis) is an inflammation of the tendon. Research has suggested little or no long-term inflammation in tendon injuries and as such the term tendinopathy is now more commonly used.
Clinical presentation of patients with tendinopathies include:
What Causes a Tendinopathy?
Tendinopathies are caused by overuse or sudden stress on a tendon. As the strain on a tendon increases, tissue damage begins. With increased stress, some tendon fibres begin to fail which results in micro-tearing and ultimately tendon failure occurs.
How Can Physiotherapy, Chiropractic and Massage Therapy Help with Tendinopathy?
The first line of treatment for a tendinopathy injury is conservative management. A physiotherapist, chiropractor or massage therapist can help by tailoring a rehabilitation program to progress you from pain to performance. The first aim of managing tendinopathies is often to reduce pain and inflammation (if acute/reactive tendinitis). The key factor in reducing pain is managing the load on the tendon. The patient should avoid aggravating activities and any other excessive forces put on the tendon. Other treatment methods that can help with pain and inflammation include acupuncture/dry needling, therapeutic modalities (IFC, ultrasound), soft tissue releases, taping, exercise, and anti-inflammatory medication.
Your Physiotherapist and or Chiropractor will assess you and identify any movement dysfunctions or imbalance such as joint range of motion, muscle weakness, soft tissue tightness, poor control of movement, abnormal biomechanics and training errors. The identified dysfunction can be treated with a combination of hands on manual therapy or manipulation, soft tissue release, acupuncture/dry needling, and prescription of an individualized exercise program. Education in regards to lifestyle modification and training errors such as excessive training volume, intensity, inadequate recovery, footwear leading to poor biomechanics, training surface (concrete, hills. etc.) is also imperative.
Your Physiotherapist and or Chiropractor might also suggest extracorporeal shock wave therapy (ESWT) to treat your tendinopathy. Shockwave therapy can stimulate the healing process by breaking down scar tissue, realigning the collagen fibers, and stimulating an increased blood flow to the area.
What Should be Avoided with a Tendinopathy Injury?
You should avoid pushing through pain, quick movements and continuing to aggravate the tendon. You may feel better after warming up and stretching the area but it is still not recommended that you push through pain as you are risking further tissue damage delaying the healing process. Tendons are sensitive to overload so it is important you allow a proper amount of time for the tendon to heal.
How Long Does it Take to Recover from a Tendinopathy?
Recovery times differ (few weeks up to months) depending on the cause, severity, duration, area of injury, the integrity of the tendon and compliance with a rehabilitation program. Tendinopathies often take a long time to resolve particularly if symptoms have been present for some months before presentation. It is imperative to seek a qualified health care professional to treat the tendon and correct any associated dysfunctions that may have caused the tendinopathy. If your injury does not respond to conservative management, your physiotherapist will direct you to a physician for further investigation and treatment options.
What are Some Safe Home Exercises I can do for a Tendinopathy
The development of a home exercise program for an individual with tendinopathy requires clinical reasoning with consideration of the diagnosis and the functional requirements of the person. Exercise prescription will vary considerably depending on the site of the pathology (insertional or mid tendon), stage of tendinopathy (reactive or degenerative), functional assessment, contributing issues throughout the kinetic chain, and exercise/sport demands.
Once the pain has settled one of the goals of the exercise program will be to improve strength and function. Depending on your unique needs (ie. sport requirements) a physiotherapist will tailor the exercise program with the goal to gradually increase the load on the muscle and tendon while monitoring pain. Tendinopathy loading programs can include eccentric strengthening (loading as the muscle lengthens), combined (isometric, concentric and eccentric) or slow resistance training. Eccentric exercises have been considered the gold standard for many years, however, including the concentric phase of exercises is important too!. An example of eccentric loading involves slow lengthening muscle contractions such as the heel drop for the treatment of Achilles tendinopathy or wrist curls for tennis elbow:
If you are suffering from tendinopathy and would like to see one of our experienced physiotherapists, chiropractors or registered massage therapists, please contact us today.
Pre and Post-Surgical Rehabilitation
If you have an upcoming surgery, how you “prehab”, prepare and strengthen before surgery, and how you rehabilitate after surgery will have a tremendous effect on a successful outcome. Success can mean different things, to you it may mean getting back to high-level sport, or simply getting through surgery with the least amount of pain during recovery and everything in between. At Sunup Physiotherapy we have experience treating an array of orthopedic surgeries like rotator cuff or labral repairs, post fractures with plates, pins and screws, total knee replacement, total hip replacement, and ACL reconstructions but also treating non-orthopedic surgeries such as C-Sections, or abdominal surgeries.
How can Physiotherapy, Chiropractic and/or Massage help with Before Surgery “Prehab”?
Before surgery, your clinician will perform a thorough assessment to determine your current state, looking at things such as strength, mobility, muscle tone, and pain levels. Taking into consideration your current abilities, an exercise program will be designed to prepare your body for what is to come. Usually, exercises would include some mobility and strengthening, along with an individualized home program. You may benefit from shockwave therapy and manual therapy to help with stiff joints at or around the area, tight muscles, or simply for pain management. Having pre-op treatment can also help with decreasing anxiety that often comes with surgery, your practitioner will be able to address all your questions and guide you in the process. The more knowledgeable you are going in the better you will feel on the other side.
How can Physiotherapy, Chiropractic and/or Massage help After Surgery “Rehab”?
After surgery, the early days of treatment are some of the toughest and treatment will focus on pain management, decreasing swelling and starting to get the body part moving with range of motion and gentle stretches. Muscle activation and soft tissue work will be important in these early days as well. The incision/scar is also something that practitioners will work on to help with healing and mobility. As pain, swelling, and mobility improves progressive strengthening often becomes the focus of rehab. The strengthening exercises you get in the early days are not the ones that will get you back into your sport or hobbies. Throughout treatment, your exercises will be designed based on your individual characteristics and what you want to get back to. Various manual therapy techniques can be performed along the way if any speed bumps arise throughout the rehab process.
What to Avoid Before and After Surgery?
Doing nothing! The worst thing you can do leading up to a surgery or after surgery is nothing at all. The weaker you are before surgery the harder it will be and the longer it will take to build up strength after surgery. The less mobility you have before surgery the longer it will take to get the mobility back after surgery. Simply resting after surgery is rarely the way to go. It could prolong pain and will not get that mobility and strength back and will not get you doing what matters to you!
When Should you Start Rehab Post Surgery?
If you know you have surgery in a couple months, it is a great time to check in with a Physiotherapist, Chiropractor or Massage therapist. Strength gains can take 6-8 weeks to start building so the earlier the better once you know you have a surgery date. Most of your prehab will be able to be done at home at this point with occasional check-in appointments to progress exercises and perform some manual therapy as needed. If you just found out you are having surgery and it is coming up in a couple of weeks it is not too late to start prehab. It can be very helpful to learn what to expect after surgery and get started on a few exercises that will start getting your muscles firing. If you are dealing with pain before surgery your therapist will also be able to provide treatment to help with pain.
The timeline to start rehab after surgery will depend on your surgery and the surgical protocol you may have been provided by the surgeon. Most orthopedic surgeries will have you start rehab within the first week of surgery.
How Long Do You Need Rehabilitation Treatment After Surgery?
How long rehab lasts will depend on your surgery but with some of the big surgeries like rotator cuff repairs and ACL reconstruction you will be working on rehab for a good 6-9 months. Treatments will be more frequent in the beginning and will slow down to roughly once a month toward the end of rehab. Usually getting the strength and agility to return to sport is what takes the longest.
If you have an upcoming surgery or have had surgery and are looking for expert post-operative care our Physiotherapist, Chiropractors and team at Sunup Physiotherapy are here to help! Contact us today.
Stress Fractures
What is a Stress Fracture?
A stress fracture is a common sports injury that can appear to come out of nowhere. It can affect people of all ages and activity levels, though it is generally associated with an increase in activity or repetitive activities. A stress fracture occurs when the body does not have sufficient rest, or building blocks (nutrients), to repair bone that is broken down during activity. This can result in pain with activity, local swelling and tenderness. The pain comes on gradually, and is usually relieved with rest. If the stress fracture worsens, the pain will also worsen and begin to appear in regular daily activities, sometimes even becoming chronic pain (>6 weeks). The most common location for a stress fracture to occur is in the foot or ankle.
What Causes a Stress Fracture?
The main cause of stress fracture is repetitive activities without proper rest periods or gradual load. When a bone is repeatedly stressed in the same way, it breaks down. If the body has sufficient rest, this cyclical process is completed and the bone is built up again (about 48hrs). If there is not sufficient rest, or there is not sufficient calcium in the body, the bone weakens in that area, forming tiny cracks that can progress to fractures through the thickness of the bone.
Who is at Risk for a Stress Fracture?
Anyone who has a recent increase in activity is at risk for a stress fracture. If you are a runner who has recently upped your mileage, have just decided to get in shape and have gone from zero workouts per week to boot-camp class five nights a week, or have commenced an intensive sport training program, you may be at risk. Women are also more at risk than men, especially if their menstrual cycle is irregular. This can be a sign of a calcium deficiency, and calcium is an essential building block for bone. Even sports like soccer, tennis, and basketball can put people at risk for a stress fracture.
What are the Symptoms of a Stress Fracture?
Since stress fractures come on gradually, the symptoms do as well. Initially there can be pain with the offending activity which is relieved with rest. As the tiny cracks in the bone increase in size, the pain can become more intense, and can be felt during regular activity as well as sporting activity. If left untreated this can progress to chronic pain. The pain is usually well localized to the injured area, and can be accompanied by point tenderness and mild swelling.
What to do if you Think you have a Stress Fracture?
The most important step is to get the right diagnosis. An appointment with one of our registered physiotherapists and/or chiropractors will determine the issue at hand. Further imaging ordered by your family doctor may be required to confirm the diagnosis. Since stress fractures are usually very small they may not show up on an X-ray, additional imaging such as an MRI or a Bone Scan may be required to confirm the diagnosis.
Physiotherapist and Chiropractic Treatment for Stress Fractures
The main treatment for stress fractures is rest. If there are underlying cause of bone weakness your doctor may prescribe medication, or have you see a registered dietitian to ensure you are providing your body with the required building blocks for your bones. If the fracture has progressed, a brace, walking boot, or crutches may be required to allow the bone time to heal.
Physiotherapy or Chiropractic care may be required to create an individualized strengthening program to reduce stress on the area. They can also help with joint mobilizations above and below the injury site to ensure proper movement and force dispersion in the area.
How to Treat a Stress Fracture at Home?
Once diagnosed you can try the following steps to aid in your recovery:
Rest
It is going to be important that the area get sufficient time for the bone to heal. You are going to have to stop painful activities and if every day activates are painful, like walking, you may need to protect the area with a brace or walking cast. If your symptoms are this severe to brace it is important to be assessed by a medical doctor. The normal duration should be around 6 weeks.
Re-evaluate and Possibly Change your Lifestyle Habits
Make sure you are eating right, getting lots of sleep and balancing your activities with rest.
Maintain Strength and Flexibility Above/Below the Area
For example if you have a stress fracture in your foot. You may not be able to do exercises around the site (especially in weight bearing) but you should be able to build or maintain core, hip and lower leg strength along with flexibility.
How Long does it take to Recover from a Stress Fracture?
Once you have been properly diagnosed and taking the correct action your recovery should take 6-8 weeks for the bone to complete a healing process. You will also need to gradually re-introduce that aggravating activity.
A stress fracture is a serious injury and if you think you may have one it is important you seek professional help from our trusted physiotherapist and/or chiropractor contact us today.
Treatment of Bursitis
What is Bursitis?
Bursitis is a commonly diagnosed injury that occurs around many joints of the body, most common in shoulder, hip, elbow and knee. It can be confirmed with diagnostic ultrasound however your trusted Physiotherapist or Chiropractor can successful treat it without the need for imaging. Bursitis meaning “inflammation of the bursa” happens when a small fluid filled sac (the bursa) that is placed in areas of high friction becomes overused and irritated. The purpose of a bursa is to help lubricate joint tendons. In this injury, the demand and friction on the bursa is too high and an inflammatory process results. This leads to painful movement or loading of the joint as the specific area is extra sensitive to compression. Warmth, redness and swelling over the area is also apparent in early stages.
How will Bursitis be Treated by a Physiotherapist or Chiropractor?
Your trusted Physiotherapist and Chiropractor will perform an assessment of the joint and the surrounding areas to confirm the diagnosis and ensure your treatment will address the reason the bursitis happened in the first place.
A Physiotherapist can apply therapeutic modalities such as Ultrasound and give you advice to help control the inflammation. Both your Physiotherapist and Chiropractor can provide manual and manipulative therapy, exercises, shockwave therapy, acupuncture and or dry needling treatment. Soft tissue release may also be indicated which can be managed through manual therapy by your physiotherapist or alternatively, they can refer you to a registered Massage therapist to help with this aspect of your rehabilitation plan.
Best Exercises to Help with Bursitis?
In the case of Bursitis, there is most likely a muscular imbalance around the joint affected. Resolution of the symptoms will typically occur once you rebalance this, by stretching what is short and tight while strengthening what is weak.
Strengthening the core and the specific joint stabilizers for endurance and motor coordination will be one goal. In conjunction with the other goal of stretching muscles that are tight. Ultimately, strength and restoring optimal length of the muscles will improving the alignment of the joint and prevent excessive compression of the bursa.
Example of a shoulder bursitis:
It is often important that you strengthen the rotator cuff and scapular stabilizers such as the Serratus Anterior and middle and lower Trapezius. While stretching the Pectoralis major and minor. Ultimately, working on improving the rounded and forward shoulder alignment that can lead to shoulder bursitis.
What Should be Avoided with Bursitis?
If you suspect or have been diagnosed with bursitis it is important that you reduce the inflammation so that healing can progress. To make sure this happens quickly play close attention to what aggravating movements or postures that may have brought it on in the first place and modify or avoid them.
Make sure you avoid putting extra pressure on the area, for example if you have shoulder bursitis avoid sleeping on it or putting weight through your arms when sitting (i.e. leaning heavily on your arm rest).
What You Can Do at Home to Help Treat Bursitis?
Your exercises will be based on the joint affected, area and cause of your bursitis, but for now here are some helpful tips to help resolve your pain.
In an acute stage, it is important to apply ice to control the inflammation. You can apply ice with compression for 10 mins 3 times a day.
Balance rest with activity. Your initial reaction to the acute pain of bursitis is going to be rest. Rest will help but if that is all you do you will never be able to get back to a pain free normal joint. So, in the early stages balance rest with activity by performing pain free range of motion exercises with the joint. Remember, you know your body best, so the ratio of rest to activity is will be best on what feels right for you.
In later stage bursitis, it is important that you are performing a daily exercise regime that is targeting the cause of the underlying muscular imbalance. Consult with our trusted Physiotherapist or Chiropractor for a personalized treatment program.
How Long Does It Take to Recover from Bursitis?
If you manage to recognize the symptoms and get control of the inflammation quickly you will have a faster recovery. In this ideal scenario, it should take 6-8 weeks for you feel fully recovered. However, you also have to make sure that you do not cause the inflammation to return or you will be delaying your recovery time. You can do this by modifying your lifestyle to avoid aggravation and completing a daily strengthening and stretching regime.
If your injury is difficult to get control over in the early stages, it can take much longer to recover and even up to a few months before you reach injury free status. This injury can be stubborn especially because once the initial irritation goes away you may not be reminded to complete your exercises. It is important that you keep consistent with them and progress them with the guidance of your physiotherapist or chiropractor for a few weeks even after the initial pain is resolved so that you prevent this issue from returning again.
If you think you may have bursitis or have been diagnosed with bursitis but can’t seem to beat the cycle of pain we encourage you to find a trusted Physiotherapist or Chiropractor. It would be our pleasure to help you if you are in the north Edmonton and need help. Contact Us today.
Joint Dislocations
What is a Joint Dislocation?
A joint dislocation is when the articulation between two bones becomes separated. When a joint becomes dislocated, the joint becomes very painful and is usually accompanied by muscle spasms, lack of range of motion and deformity. Muscle spasms occur when the body attempts to maintain stability at the joint. A person who dislocates a joint should seek medical care at the local hospital and may undergo a joint reduction procedure (when the structure is brought back to its normal anatomical position). Further investigations such as imaging may be required to rule out fractures or injury to a nerve.
What Causes Joint Dislocations?
Joint dislocations are caused by the following:
How Can Physiotherapy or Chiropractic Help with a Joint Dislocation?
While it is not in a physiotherapist or chiropractor’s scope of practice to reduce a dislocated joint, both can help you rehabilitate the joint after your injury has occurred. Your physiotherapist or chiropractor may use various modalities such as shockwave therapy, ultrasound, laser, ice and interferential current to help decrease joint swelling/inflammation, promote healing and decrease pain. Your physiotherapist or chiropractor may perform various manual therapy and soft tissue techniques to help reduce pain and gradually increase range of motion. Most importantly, they will identify the root cause of the dislocation and address any muscle imbalances by teaching you specific exercises tailored to your condition.
What Should be Avoided with a Joint Dislocation?
When a joint has become acutely dislocated, it is not recommended for the person to attempt to self-reduce the joint. It is advised that the person seek medical help at the hospital. Any activities that caused the dislocation should be avoided until cleared by a medical professional to prevent repeated episodes. Your physiotherapist or chiropractor will guide you through the process of returning to activities or sport.
How Long Does it take to Recover from a Joint Dislocation?
The recovery time for a joint dislocation is variable and can take weeks to months to fully resolve. It is also crucial to rehabilitate the joint to ensure prevention of future episodes of dislocation. If a joint repeatedly dislocates, it is recommended to seek a consultation with an orthopedic surgeon. This requires a referral from your family doctor.
What are Some Safe Home Exercises I can do for a Joint Dislocation?
Your Physiotherapist or Chiropractor can help determine the most appropriate exercises for you. Management and exercises may include:
If you are suffering from a joint dislocation and would like to see one of our registered physiotherapists or chiropractors, contact us today.
What is Osteoarthritis?
What is Osteoarthritis?
The word arthritis means inflammation of the joint. While there are many different types of arthritis, osteoarthritis (OA) is the most prevalent form, and it affects so many Canadians.
In a joint affected by arthritis, the cartilage (a flexible connective tissue which covers and protects the ends of bones) begins to wear down. Cartilage is very important for a joint to function well; it helps absorb shock and allows for smooth movement between bones. When the cartilage wears down in osteoarthritis, this often results in pain, stiffness (especially in the morning), and swelling. Over time, joints affected by osteoarthritis may slowly become bigger, and in severe cases the cartilage may wear away completely and the bones may rub together causing even more pain. The symptoms of pain and stiffness associated with osteoarthritis often cause the joints to be used less often, which ultimately leads to a weakening of the muscles around the joints. This then becomes a negative cycle because if the muscles are weaker, they are less able to provide support for the joints resulting in increased pressure through the boney surfaces.
What Joints are most Commonly Affected by Osteoarthritis?
What are the Signs and Symptoms of Osteoarthritis?
Osteoarthritis usually progresses slowly over a period of months to years. Below are some common symptoms you may experience.
What are the Risk Factors for Developing Osteoarthritis
Some risk factors for developing osteoarthritis include:
We do not yet know the cause of OA and there is currently no cure for this condition. However, we do know some factors that can put an individual more at risk of developing OA and some of these factors are under our control. We also have many options to help manage OA in joints that have already developed it including physiotherapy and chiropractic care. It is important to keep the muscles around the joint strong and active.
What do you do if you think you have Osteoarthritis?
If you think you might have OA, it would be a good idea to discuss this with your family doctor. They will be able to assess your symptoms and send you for any X-rays they deem appropriate to help with a diagnosis. If your doctor believes you have OA, they will educate you on treatment options including medications, physiotherapy or chiropractic care and surgery in severe cases.
How can a Physiotherapist or Chiropractor Help with Osteoarthritis?
Physiotherapy or Chiropractic are excellent treatment options for people with osteoarthritis. They can help control your pain and maximize your function to optimize your quality of life.
Some of the key components of a physiotherapy or chiropractic intervention for osteoarthritis are:
Exercise
Your physiotherapist and/or chiropractor will prescribe specific exercises and stretches to help maximize the range of motion and flexibility in your affected joints. They will also show you exercises to strengthen the muscles that can help protect and support your joints. Your physiotherapist may also recommend some form of low impact exercise, which can help manage your symptoms of pain and stiffness.
Other Therapeutic Modalities
Physiotherapists are skilled in the application of many other modalities which can make a big difference in reducing pain and swelling associated with arthritis. Such modalities include shockwave therapy, ultrasound, laser, interferential current (IFC), TENS, acupuncture, dry needling / IMS.
Manual Therapy
Physiotherapists and Chiropractors are experts in using manual therapy for both joints and soft tissues to help modulate pain and increase range of motion.
Custom Knee Bracing for Osteoarthritis
Our trained physiotherapists can measure you for custom knee braces to help with osteoarthritis. We offer the DonJoy Defiance III brace which is highly effective and can help to off load the compartment of the knee affected so you can experience less pain with day to day activities. There are other off the shelf braces that can also help protect your joint and give it support it needs so that the pain can settle and you can begin to strengthen the area.
How can you Manage Osteoarthritis at Home?
Heat and Ice
Applying heat or ice to affected joints can help relieve local pain. Heat is specifically good for relieving muscles spasms and tightness, as well as promoting range of motion. Ice is specifically good for decreasing swelling and constricting blood flow to an already inflamed joint.
Joint Protection
A physiotherapist or chiropractor will educate you about ways you can reduce the stress on your joints with daily activities. Some strategies include:
Things you can do to Avoid Developing Osteoarthritis?
If you have osteoarthritis and are interested in learning more about how a physiotherapist or chiropractor can help you reduce your pain and maximize your function, contact us today.
Calcific Tendinitis
What is Calcific Tendinitis?
Calcific tendonitis – Calcium deposits in tendons that commonly occur in the shoulder rotator cuff causing pain, irritation and inflammation in the area. Most often found in the supraspinatus, infraspinatus and subscapularis tendon.
What Causes Calcific Tendinitis?
Calcific tendonitis is one of the most common causes of non-traumatic pain in the shoulder. However the underlying causes are still poorly understood.
The following list has been identified as possible causes
Clinical Presentation of Calcific Tendonitis
Depending on the stage of the condition, you may experience different signs and symptoms.
Pre calcification phase
Minimal to no pain, but cellular changes predisposing the tendons to developing calcific deposits
Calcific phase
3 substages
1. Forming of calcific deposits (no pain or pain with movement only
2. Resting phase (no pain)
3. Reabsorption (most painful, typically lasting 2 wks)
Post Calcific Phase
Variable symptoms, deposit reabsorbs, and replaced by regular tissue. May lasts for months
The chief complaints:
Differential diagnosis may be needed, as some of these symptoms may be indicative other shoulder pathologies, such as rotator cuff tears and adhesive capsulitis. Our physiotherapists and chiropractors can perform a thorough assessment to determine the best course of treatment.
Treatment of Calcific Tendonitis
Conservative
According to literature, about 90% of people with the condition are successfully treated without surgery. There are a number of treatment options available to treat calcific tendonitis.
Shockwave therapy
Shockwave therapy improves symptoms of calcific tendonitis resulting in decreased pain and improved function and use of the joint.
Shockwave uses focused high frequency sound waves directed to the affected tendon. The exact mechanism of action on calcific tendonitis is unknown. It is theorized that it prompts a tissue response in order to absorb the calcium deposit. More recently it has been suggested it also has a role in affecting the neural processes involved in pain memory leading to permanent healing instead of a temporary fix.
To read more about shockwave therapy, please read.
Manual therapy
Manual therapy can help regain movement by mobilizing soft tissue (muscle and fascia) and the joint capsule. It also aids in modulating pain, reduces soft tissue swelling, restore muscle function, and induces relaxation.
Exercise therapy
Individualized targeted exercise therapy that aims to decrease pain, restore range of motion, shoulder and scapular strength has been found to improve symptoms.
Load and capacity management
Proper load and capacity management is the cornerstone of optimal recovery. When a tissue is loaded beyond its capacity injuries can occur. During the rehabilitation process the goal is to improve tendon capacity with progressive loading.
Physiotherapists can help you manage gradual exercise progressions, and give you suggestions how to temporarily modify certain activities.
Surgery/Excision
Some cases are resistant to conservative treatment and surgery may be a viable option for them. Following surgery, a course of physiotherapy rehabilitation is recommended for the best results.
If you have shoulder pain and would like to improve your symptoms, book an appointment with one of our physiotherapists. Contact us today to set up an initial consultation.
Osteoporosis Management
It’s only natural to have questions, concerns and to wonder, how exactly you can continue to live a happy and healthy lifestyle after an osteoporosis diagnosis. Read on to learn about potential risks and how you can manage your new diagnosis to prevent fractures.
What is Osteoporosis?
Osteoporosis, known as the “silent thief”, is a disease characterized by an asymptomatic decrease in bone mass. Bones become thin and porous, reducing their strength and leading to an increased risk of fractures. Both women and men can be affected by this disease and it can strike at any age. By our mid-30s both women and men begin to loose bone mass, and the rate of loss increases for women after menopause. Although there is no single cause for osteoporosis there are certain risk factors including: age, sex, a loss of height greater than 2cm (indicating potential degenerative changes in your spine) a history of a bone fracture from a fall while at standing height after the age of 40 or a family history of the disease.
There is also a prevalence of secondary osteoporosis. This is characterized by a loss of bone mass occurring as a result of another disease or treatment that affects bone health. Often certain medications have been linked to a loss in bone mass, for example, synthetic glucocorticoids, breast and prostate cancer drugs, heart burn drugs and blood pressure drugs to name a few. Certain medical conditions such as rheumatoid arthritis, malabsorption syndromes and sex hormone deficiencies have also been linked to bone deterioration.
What are the Risks if I have been Diagnosed with Osteoporosis?
Fractures from osteoporosis are very common. At least 1 in 3 women and 1 in 5 men will suffer from an osteoporotic fracture in their lifetime. As you can imagine this is a huge burden on the Canadian Healthcare system. Bones most at risk for osteoporotic fractures include the wrist, hip and spine. Without proper intervention your bones could become more brittle, increasing your risk for fracture.
What can you do to Manage your Osteoporosis and Prevent Fractures?
Once diagnosed with osteoporosis your doctor will be able to provide you with guidance on both your nutrition and whether you are a candidate for drug treatments aimed to reduce fractures. You have likely heard how important calcium and vitamin D are for bone health. A well balanced diet is a powerful tool to fight the further degeneration of your bones. Speak with your family physician or a dietician to ensure your diet is rich in these essential nutrients to maintain your bone health.
We all know that exercise is an important part of a healthy lifestyle, but did you know it can also be an essential part of building and maintaining your bone health? To pursue a safe exercise program be sure to review with your physician or a Physiotherapists your risk of fracture. From there a Physiotherapist can help you design an exercise program tailored to your needs. Weight bearing exercises to improve bone strength, strength training to improve posture and mobility, as well as balance training to reduce the risk of falls are all key elements in an exercise program tailored to improve your bone health!
Contact us today if you have been diagnosed with osteoporosis and would like any of our trusted physiotherapists to provide more education on the disease and an exercise program tailored to reduce your risk of fracture and improve your bone health.
What is chronic pain and how do we treat it?
Sharp, dull, achy, burning, radiating, shooting these are just some of the ways patient’s have described their pain. Pain is one of the main reasons why patient’s come to see us. Whether from an acute injury, a surgery or something that came out of the blue, pain is often what drives us to seek help! Pain is actually a good thing! It grabs our attention and warns us of an actual or potential threat to our body’s tissues, helping to protect us from further damage. However, sometimes our body’s alarm system doesn’t stop ringing the alarm even after source of harm is gone. What is happening when our tissues have healed, our injuries have repaired but the pain has not?
Chronic pain is defined as any pain that lasts greater than 3 months. This is the amount of time that it takes tissue from an acute injury to heal. To understand chronic pain we must first understand how we perceive pain.
Pain and in turn chronic pain, is multifactorial. Not only can a sensitized nervous system affect how you perceive pain but your emotional well-being and your thoughts and beliefs about pain can also influence your pain experience. An encounter with a stimuli that was previously perceived to be painful can provoke a sense of fear or anxiety in someone. These feelings can have a direct effect on our physiology, increasing the production of cortisol and other stress hormones which can themselves lead to sensitization of our peripheral and central nervous system
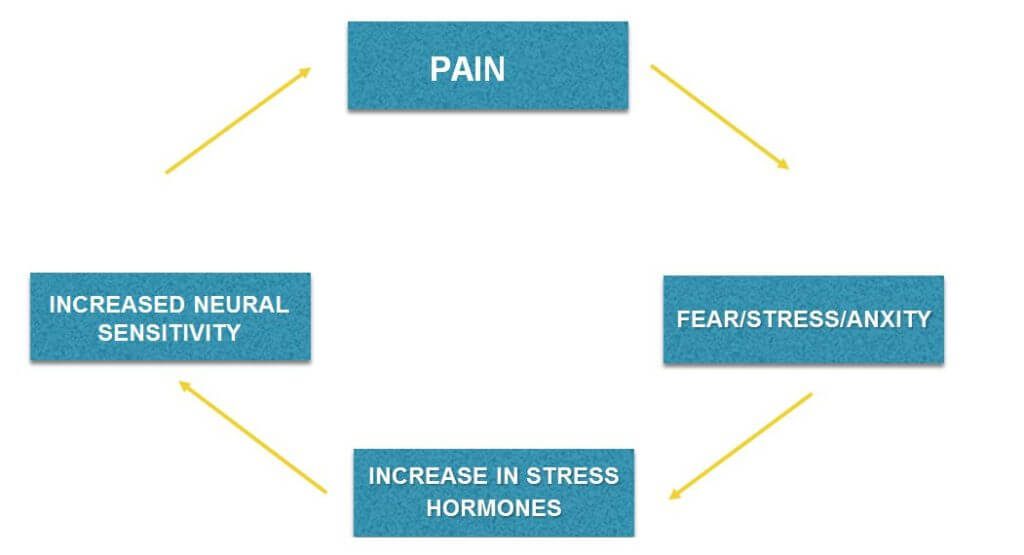
So how do we treat something as complex as chronic pain? With a multi-factoral approach! A physiotherapist will work to de-sensitize the nervous system. This may include releasing tight muscles, strengthening weak muscles and improving neural mobility. We promote graduated return to pain free movement of the affected area, which helps to re-program our sensitized nervous system. The brain learns that not all movement is painful, minimizing fear and anxiety associated with movement and reducing the level of stress hormones sensitizing the system. Treatment may also include such tools as mindfulness, meditation and body mapping to help patients gain control of their negative thoughts and beliefs about their body and the pain they are experiencing.
The research behind pain science continues to grow and we learn more about managing chronic pain every day. If you suffer from chronic pain, contact us today to book an assessment with one of our trusted physiotherapists!
Pregnancy and Pelvic Floor Physiotherapy:
Prehab for Labour!
Pregnancy can be an exciting and sometimes overwhelming 9 months as your body grows and changes as you prepare to bring a new life into this world. From the multiple visits with your healthcare provider, the prenatal classes and preparing your home for the arrival of a new family member it can be a very busy time. Many patients question whether they should have a pelvic physiotherapy examination during their pregnancy, particularly if they aren’t having any symptoms?
A common misconception about pelvic physiotherapy is that it really only helps after labour, in the postpartum period to address problems that can arise. This just isn’t true! In the same way we work with patients training for a marathon or our athletes preparing for the big game we can help you prepare for the challenges you might face during pregnancy and labour!
So, what exactly can pelvic physiotherapy help with?
Exercise and Pregnancy
An exercise program (cardiovascular exercise) during pregnancy has been associated with a shortened stage one and stage two labour. Whether you already have an exercise program that you want to continue with or you want to become more active during your pregnancy, your pelvic physiotherapist can help with the following:
Pelvic Girdle Pain
Pregnancy related pelvic girdle pain is described as any pain experienced in the pubic symphysis (front of the pelvis) or sacroiliac joints (low back) during pregnancy. Pain is often reported as early as 14 weeks gestation and as late as 30 weeks, with as high as 60-70% of women reporting some pelvic girdle pain by late pregnancy. What many women don’t know is that pelvic physiotherapy can help to make you more comfortable throughout your pregnancy and reduce or even eliminate your pelvic girdle pain. Treatment may include:
Address Urinary Incontinence (Leakage)
Pelvic physiotherapy is often associated with addressing urinary incontinence or leakage that can occur after a vaginal delivery, but if you start to experience urinary incontinence during pregnancy it is important to address it! Strengthening in the prenatal period has been shown to help to prevent stress incontinence in the postpartum period. That means pelvic floor strengthening can be preventative when performed throughout your pregnancy 4.
Labor Prep
So, think about physiotherapy during pregnancy as your prehab for labour and the postpartum period!
Contact us today if you would like one of our pelvic physiotherapists to help you prepare for pregnancy.
Hypermobility Syndromes
What is a Hypermobility Spectrum Disorder?
Hypermobility Disorder (HD) is an umbrella term that generally describes someone who has hyper mobile joints with symptoms. A hyper mobile joint is not a disease or a diagnosis. It simply describes a joint that moves a greater than average range of motion. It becomes a disorder when it starts to cause symptoms such as pain, instability, impedes function and activity.
What Causes a Hypermobility Disorder?
There are a number of factors that determine the stability and mobility of a joint. Examples include – the shape of the bones, training, previous injury, muscle strength and proprioception (how we perceive the position and movement of our joints). Other factors include genetics, age, gender and hormones.
A HD may or may not be associated with an underlying Connective Tissue Disorder (CTD). Connective tissue makes up some of the major structures of our body – our muscles, bones, ligaments, blood vessels, gastrointestinal system etc. With a CTD there are changes in the strength and laxity of connective tissue throughout the body. Examples of these include Ehlers-Danlos Syndrome, Marfan Syndrome, Loeys-Dietz Syndrome. An individual will likely have hyper mobile joints and other symptoms throughout the body as well.
What are Signs and Symptoms of a Hypermobility Disorder?
An individual with a HD will have one or more hyper mobile joints throughout their body. Their elbows and knees may hyperextend or their fingers can bend backwards quite far. Any joint in the body can be affected. These joints may also be painful and lack control.
Other common symptoms include: headaches/migraines, abnormal skin – skin that stretches far or scars easily, anxiety, gastrointestinal problems – bloating, constipation, early satiety, fatigue and pelvic organ prolapse.
Frequently these individuals will also have disturbances in their autonomic nervous system and may experience something called Postural Orthostatic Tachycardia Syndrome (POTS). With POTS a persons heart rate will increase abnormally with position changes. A person may feel light-headed, fainting spells, blurred vision, blacking out with changing position.
Are you Hypermobile?
Try answering the 5 questions below:
- Can you now (or could you ever) place your hands flat on the floor without bending your knees?
- Can you now (or could you ever) bend your thumb to touch your forearm?
- As a child, did you amuse your friends by contouring your body into strange shapes or do the splits?
- As a child or teenager, did your shoulder or kneecap dislocate on one or more occasion?
- Do you consider yourself “double-jointed”?
If you answered “yes” to two or more of these questions it suggests that you have generalized joint hypermobility.
How is a Hypermobility Disorder treated?
A physiotherapist or chiropractor at Rebalance will assess the range of motion and stability of the joints throughout your body. After that assessment they will teach you how to activate deep stabilizing muscles surrounding your affected joints. They will teach you how to maintain your joints in a neutral and safe position. You will be given a tailored exercise program that focuses on improving your strength, balance and position awareness. They will also treat any painful joints and muscles with manual therapy and other modalities.
For more systemic symptoms, you may also see a pelvic physiotherapist if you are experiencing any pelvic problems. If you are experiencing any dysautonomia symptoms (i.e. POTS) the best treatment for this is a specific exercise program focused on controlling position changes, compression stockings and diet changes.
If you have been diagnosed with a Hypermobility Disorder or are concerned about the stability of your joints definitely set up an assessment with one of our healthcare professionals. There are lots of fully functional, high level athletes with extremely hypermobile joints. With a couple tips and tricks, we can get you back to whatever activity or sport you love to do! Contact us today to get help!

